What is Tibial Interlocking Nail and How Does it Work?
The Tibial Interlocking Nail is a critical tool in orthopedic surgery. Dr. Emily Carter, a renowned orthopedic surgeon, states, "The Tibial Interlocking Nail revolutionizes how we repair fractures." This innovative device stabilizes fractured tibias, allowing for enhanced healing.
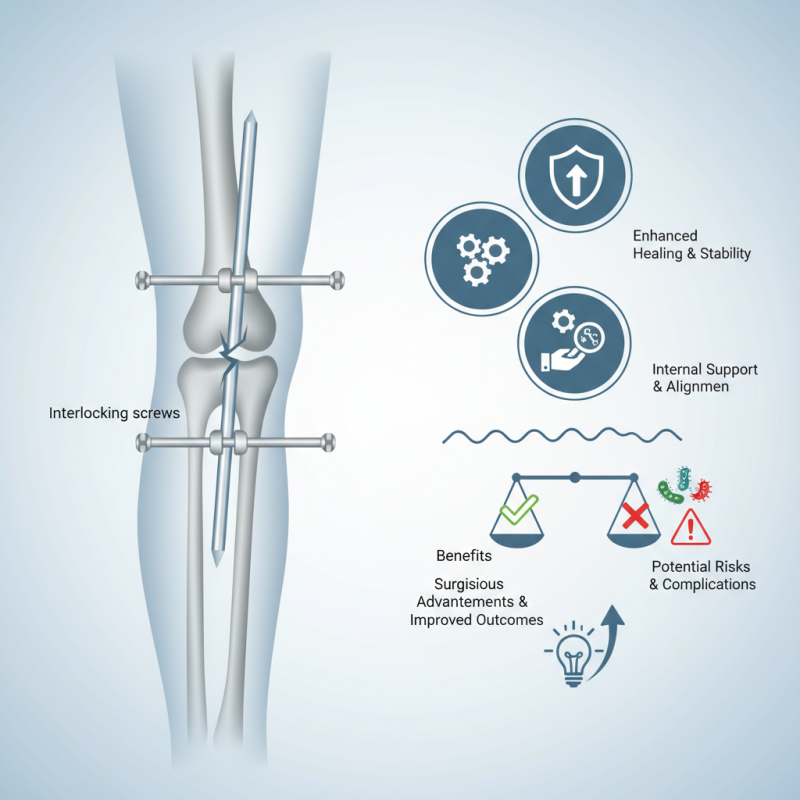
This nail provides an internal structure to support the bone. It features interlocking screws that ensure proper alignment during recovery. These design elements promote faster and more efficient healing for patients. However, there are complexities involved in its application. Each case demands careful consideration of the patient's unique anatomy.
Despite its advantages, some challenges remain. It's essential to monitor for complications, such as infections. Surgeons must weigh the benefits against potential risks. Continuous advancements in techniques and materials are necessary for better outcomes. The Tibial Interlocking Nail has changed orthopedic practices, yet ongoing discussions and reflections are vital to improve patient care.
What is Tibial Interlocking Nail?
The tibial interlocking nail is a surgical implant used to stabilize fractures in the tibia, the shinbone. This device allows for a strong fixation, ensuring proper healing of the bone. It is inserted through the medullary canal and secured with locking screws at both ends. This design helps to resist rotational forces, enhancing stability. According to recent studies, this method has a success rate of over 90% in promoting bone healing.
Tips: Proper alignment during insertion is crucial. Misalignment can lead to complications. Surgeons should ensure the correct technique is applied. Monitoring the patient's recovery is equally important, as timely interventions can prevent further issues.
The effectiveness of the tibial interlocking nail lies in its versatility. It can be used for various fracture types, making it a preferred choice among orthopedic surgeons. Data from orthopedic journals indicate a decrease in malunion rates when this method is applied. However, challenges exist. Some patients experience complications, such as infection or delayed healing. Continuous evaluation of patient outcomes is essential for improving techniques.
Indications for the Use of Tibial Interlocking Nail
Tibial interlocking nails are commonly used in orthopedic surgery. They play a vital role in stabilizing tibial fractures. However, knowing when to use them is essential for optimal recovery.
Indications for the use of tibial interlocking nails include complex fractures. This can involve multiple fracture lines or unstable fragments. They are particularly useful in cases with diaphyseal fractures, which are located in the shaft of the bone. When treating these injuries, surgeons consider the patient's age and activity level.
Infections or poor bone quality may complicate the decision. This requires careful assessment and planning. Tibial interlocking nails also allow for early mobility, promoting faster healing. But not every fracture benefits from this method. Surgeon experience and patient specific details matter greatly. It's a delicate balance to strike. Each case may present unique challenges.
The Surgical Procedure for Tibial Interlocking Nail Insertion
The surgical procedure for tibial interlocking nail insertion involves several important steps. First, the patient is positioned on the operating table. Proper anesthesia is administered for comfort. Surgeons typically make an incision near the knee or ankle, depending on the fracture site. This allows better access to the bone.
Next, a drill is used to create a hole in the tibia. The interlocking nail is then carefully inserted into the canal. Precision is key here. Surgeons must ensure the nail is aligned correctly. Misalignment can lead to complications, such as improper healing. After placement, locking screws are inserted through the nail. This stabilizes the fracture.
Monitoring during the procedure is critical. Surgeons watch for excessive bleeding or damage to surrounding tissues. Post-operation, patients often need rehabilitation. They may find it challenging to regain full mobility quickly. Recovery can be slow and frustrating. Regular follow-ups are necessary to ensure proper healing.
What is Tibial Interlocking Nail and How Does it Work? - The Surgical Procedure for Tibial Interlocking Nail Insertion
| Dimension | Details |
|---|---|
| Procedure Name | Tibial Interlocking Nail Insertion |
| Indications | Tibial fractures, unstable fractures |
| Surgical Approach | Intramedullary insertion through the knee |
| Anesthesia Type | General or regional anesthesia |
| Duration | 1-2 hours |
| Recovery Time | 6-12 weeks for full recovery |
| Complications | Infection, non-union, malunion |
| Post-operative Care | Rehabilitation exercises, pain management |
Mechanism of Action: How Tibial Interlocking Nail Stabilizes Bones
The Tibial Interlocking Nail is a surgical device. It is used for stabilizing fractures in the tibia, or shinbone. Understanding its mechanism of action is crucial for its effective use.
This device works by being inserted into the medullary cavity of the tibia. Screws are placed at various angles to secure the nail. This helps maintain proper bone alignment. The nails support the bone during the healing process. They allow for weight-bearing earlier than other methods.
Tips: After surgery, following rehabilitation is vital. Engage in physical therapy to strengthen the area. Listen to your body. If pain persists, consult your doctor.
The design of the Tibial Interlocking Nail allows for enhanced stability. However, improper placement can lead to complications. It is essential for the surgeon to have extensive experience. Regular follow-ups are crucial for monitoring recovery.
Postoperative Care and Rehabilitation for Tibial Interlocking Nail Patients
Postoperative care for patients with a tibial interlocking nail plays a crucial role in recovery. After surgery, patients typically require immobilization. This often involves using crutches to avoid putting weight on the affected leg for approximately six to eight weeks. Early mobilization can be beneficial, but it should be pursued with caution. Rehabilitation often begins with gentle range-of-motion exercises as soon as tolerated, helping to reduce stiffness while preventing complications.
Physical therapy is essential for restoring function. Studies show that structured rehabilitation can improve strength and mobility significantly. According to a recent report, patients who engaged in targeted rehabilitation achieved a 30% faster return to full function within three months. However, individual recovery rates vary. Some may experience complications like delayed healing or infection. Regular follow-ups with healthcare providers are crucial for monitoring progress and addressing any concerns.
Patients often struggle with pain management and might feel frustrated during recovery. It's normal to have emotional highs and lows. Open communication with medical teams about these feelings is important. Many patients benefit from support groups or counseling. Engaging with others facing similar challenges can provide motivation and reassurance. Each person's journey to recovery is unique, and patience is key.

